The Future of Colorectal Cancer Prevention in Developing Countries
Vol. 18, Issue 1 (March 2013)
 |
René Lambert, MD
Screening Group
I.A.R.C, Lyon, France
|
The burden of colorectal cancer in the world
Over the world, colorectal cancer is the third most common cancer in men, and the fourth in women. In the IARC GLOBOCAN database 1 incident cases of colorectal cancer in 2008 were estimated, for both genders, at 1,234,000, out of which 727,000 are in developed countries and 506,000 are in developing countries. Colon cancer is located either in the proximal segment (ascending colon and right angle), the transverse segment and left angle, or the distal segment (descending colon and sigmoid). Rectal cancer is located distally between the recto-sigmoid junction and the anal margin.
In each region of the world the burden of colorectal cancer is estimated in population based cancer registries. Observed data in cancer registries display precise information in the fraction of population concerned. For the global population of a country estimated figures are found in the 2008 edition of the IARC database GLOBOCAN 1. Incidence, or the annual number of cases occurring in a corresponding population of 100,000 persons is expressed as an age standardized rate of Incidence (ASR)/100,000 persons which refers to a standard of distribution of age classes in the world population in 1960. This standard, adopted in the IARC monographs (Cancer Incidence in V continents 2 and GLOBOCAN 1), allows comparisons of the risk between countries having a different distribution in the age classes of the population. Mortality is the yearly number of deaths in the corresponding population of 100,000 persons. The mortality rate is also expressed as an ASR mortality/ 100,000 persons, in reference to the standard of the world population in 1960. Survival is estimated from registries having a regular follow-up of the cases included. The 5-year Relative Survival (5y-RS) takes in account the life expectancy of persons of the same sex and age, not suffering from this cancer. In addition the index of Disability Adjusted Life Years (DALY), based on incidence and mortality, includes successive steps from cancer detection to death, with the years of disability. DALY is expressed as the number of years lost/100,000 persons of the target population.
Colorectal cancer in developing countries
In geographical regions of the world, countries are also classified in reference to their development: more developed countries predominate in all regions of Europe and in North America, Australia/New Zealand and Japan. Less developed countries are found in all regions of Africa, Asia (excluding Japan), Latin America and the Caribbean, Melanesia, Micronesia and Polynesia. Some countries like Brazil, Russia, India, China, not yet classified in the more developed group, are called “emerging” because of the fast development of their resources. Country resources have been classified in four categories by the World Bank 3, according to the annual Gross National Income (G.N.I.) “per capita”, expressed in US Dollars. In 2011 the G.N.I. per capita was $1,000, or less, in the Low Income group of countries, $1,000 to $4,000, in the Lower Middle Income group $4,000 to $12,000 in the Upper Middle Income group, and more than $12,000, in the High Income group. A more precise classification is the Human Development Index (H.D.I), based on multiple parameters including G.N.I, education and years of school, health education and living standard.
1) Incidence: Considerable variations in the incidence, of colorectal cancer between regions, and countries of the world depend on causal factors in relation to development. In the GLOBOCAN, in 2008 1 the average ASR incidence of colorectal cancer for 100,000 is much higher in More Developed (30.1/100,000) than in Less Developed countries (7.1/100,000). As an example, in the more developed countries, the respective figures (both sexes) are 29.4/100,000 in France and 38.0/100,000 in Norway in Europe and 29.2/100,000 in the USA in North America, and 31.5/100,000 in Japan in Asia. Lower figures occur in the less developed countries as 14.2/100,000 in China in Asia, 6.5/100,000 in Mexico in Central America, 9.8/100,000 in Algeria, 5.9/100,000 in Uganda, and
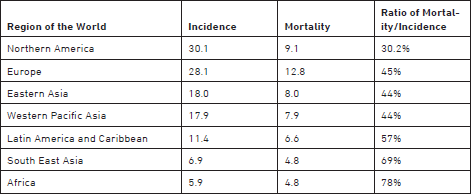
2) Mortality: In 2008, the average figure of the ASR mortality from colorectal cancer was 12.0/100,000 in the More Developed countries and 6.0/100,000 in the Less Developed countries. Mortality is related to survival of colorectal cancer, which depends on the proportion of early detection and curative treatment. The ratio of Mortality to Incidence rates is much lower in More Developed countries (39%) than in Less Developed countries (84%). The respective rates of Incidence and of Mortality in different large regions of the world are displayed in Table 1, with the ratio of Mortality to Incidence. The lowest ratio is for North America region, and the highest ratio is for Africa.
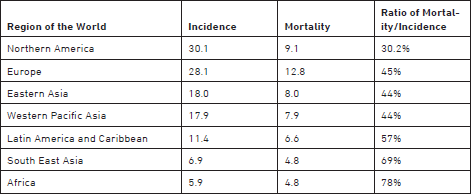
Table 1: Estimated Age Standardized rate of incidence and mortality for colorectal cancer, in 2008 in a population of 100,000 persons, for both sexes, in different regions of the world. In addition is given the ratio of the mortality to incidence rates. From IARC GLOBOCAN database in 2008.
3) Survival: In cancer registries with a regular follow-up, the five year survival of the cases included can be determined. Survival depends on the early diagnosis and proportion of cases detected at a curable stage. At the country level, survival from colorectal cancer is analyzed in period 1990-94 in the CONCORD study 4. The respective 5y-RS for men and women is high in 1990-94 in the USA at 51.9% and 60.2%, and in Japan, at 61.1% and 77.3%. Screening is developed in both countries. In contrast, the 5y-RS is low, in the range 10% - 20% in Less Developed countries of Africa where early detection is not frequent.
Causal factors of colorectal cancer
In a large majority of cases, cancer is a sporadic disease and the risk is influenced by exposure to environmental carcinogenic factors, classified as toxic, infectious and linked to diet and nutrition. This justifies a primary prevention of cancer through control of these factors connected to lifestyle and environment. Diet and nutrition play a determinant role in the risk for colorectal cancer, in relation to an excess of calories ingested with a high proportion of red and processed meat and fat. The altered diet is associated to overweight, resistance to insulin and production of insulinlike growth factors, like the IGF-1 which stimulates the proliferation of intestinal cells 5,6,7. A sedentary lifestyle with decreased physical activity is a frequent associated causal factor. In more developed countries, these factors that closely relate to the development of resources and urbanized life likely explain the higher incidence of colorectal cancer. In the UK, a European country classified in this group, the proportion of colorectal cancer attributable to lifestyle and environmental factors, is estimated at 54% in 2010 8. In Japan, an Asiatic country classified in the same group, the ASR incidence/100,000 of colon cancer increased from 8.3 in 1973-1977 to 36.0 in 1998-2002 for men, and from 7.3 to 21.5 for women. This variation correlates with ascending resources and development of a Westernized style of life.
In Less Developed countries of Africa often classified in the Low Income Group, the incidence of colorectal cancer remains low in 2008, as shown in Table 1. On the other hand, in “emerging” countries, like Brazil and China, the incidence of colorectal cancer correlates to the progression of the country income and a rapid increase is expected in relation to the progression of their resources and the urbanized style of life. However, a different situation occurs in India 9 where a spontaneous prevention is afforded by the generalized practice of a vegetarian diet, with enough physical activity; in 1998-2002, the respective figures of the ASR incidence/100,000 of colorectal cancer in men and women in the IARC database “Cancer Incidence in V Continents” were still low at 5.9 and 4.4 in the urban registry of Mumbai, and 4.1 and 3.6 in the rural registry of Karuganappally2. The incidence of colon cancer remained stable and low in the Urban Mumbai registry, during the period 1973 to 2002 in spite of the development of the city.
Perspective on evolution of the burden of colorectal cancer
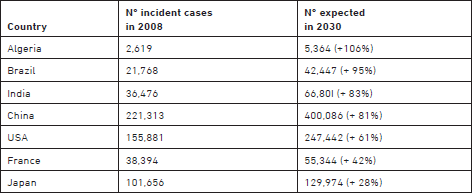
The worldwide burden of colorectal cancer will increase in the next few decades in relation to the increase in the world population and in the proportion of older age groups. An estimation of the variation expected in 2030 is given in GLOBOCAN 1: - the annual number of incident cases worldwide, in 2008 for both sexes is estimated at 1,235,198 with 59% of cases over 65 years. In 2030 the expected number of incident cases should be 2,179,771, with 65% in the age classes from 65 years. At the level of a single country the variation depends of multiple factors: 1) The structure of its population in age classes in 2008, and the birth rate; 2) The perspective in development and increased resources of the country; and 3) The strategy adopted for screening and treatment of precursors. Considerable differences occur between countries, as shown in Table 2. As a More Developed country, Japan already has an aged population, stable resources, and an established policy of screening; as a consequence, incident cases of colorectal cancer during the period 2008-2030 are expected to increase only by 28%.
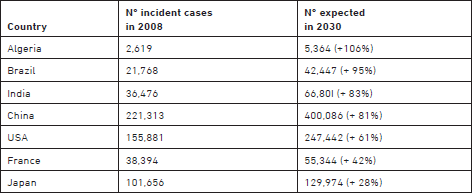
Table 2: Estimated number of incident cases occurring in 2008, in both sexes and projected number of cases in 2030, based on population growth and ageing in some countries of the world. From IARC GLOBOCAN database.
In developing countries, a major increase in the incidence of colorectal cancer is expected if they have a young population and increasing resources. In these countries a policy of prevention of colorectal cancer is justified. This applies particularly to emerging countries like Brazil, India, and China; however, in India, spontaneous primary prevention is provided by the generalized practice of a vegetarian diet with enough physical activity. In the group of emerging countries, Brazil has a relatively young population and a fast increase in resources: in 2030, incident cases are expected to increase by 95%. In conclusion, in developing countries increased income will correlate with increased risk of colorectal cancer with modifications based on variations in the nutrition and physical activity of the populace.
Perspective on screening and early detection of colorectal cancer
Primary prevention of colorectal cancer is based on a reduction of ingested calories and increase in physical activity. This prescription has an impact on weight and obesity. In perspective the control of nutrition and diet is necessary in developing or in “emerging” countries as well as in the more developed countries.
To complement primary prevention, secondary prevention aims to reduce the number of incident cases by the destruction of premalignant adenomatous precursors and early detection of cancer at a curable stage. Screening modalities for the selection of asymptomatic persons susceptible to harbor neoplastic colorectal lesions include two distinct steps: 1) A simple preliminary filter test like the detection of fecal occult blood, with an acceptable compliance and a negative or positive response; and 2) A more complex endoscopic exploration, requiring material and experience, to be performed only in persons positive to the first test. Endoscopic procedures, either with flexible sigmoidoscopy or complete colonoscopy, will confirm the presence of the lesion and eventually proceed to the resection of a superficial cancer or a premalignant adenoma.
Repeated screening trials for colorectal cancer are often offered in Developed Countries in Europe, North America and in Japan, to persons in the age range 40 to 70 years. The policy of secondary prevention deserves to be generalized in the Developing Countries. The incidence of colorectal cancer is still low in the less developed countries of the world, but the impact of delayed diagnosis and poorly adapted treatment increases the global burden of cancer, with impact on survival and mortality.
1) The Role of Health Authorities: As a rule, in each country, the prevention of cancer is under control of a National Health Service, like in the UK, or of a Ministry of Health and Family Welfare; like in India. For prevention of colorectal cancer, the National Authorities should actively encourage the control of environmental carcinogenic factors, linked to diet with excess in calories and lack of vegetables and the development of physical activity. The organization of a screening policy of secondary prevention also depends on the National Authorities. Developing Countries with low resources have not yet structured their National Health Care System. “Emerging” countries with higher resources, have already built Health Care structures and cancer control in urban areas; but heterogeneity persists with a lower impact in rural than in urban areas. In developing countries with low resources, any progress in the prevention of colorectal cancer will also require the establishment of a National Policy of Health Care.
2) The Fecal Occult Blood Test: The Fecal Occult Blood Test (FOBT), is a filter test, repeated at 2-year intervals 10. Colonoscopy is proposed to persons positive to this filter test. The global sensitivity of FOBT is around 50% for colorectal cancer and much lower, around 20%, for adenomas, with a significant proportion of false positive reactions. In spite of some debate about efficacy, the capacity of the FOBT protocol to reduce colorectal cancer mortality, has been confirmed in the period 1990-2000, by three randomized trials in the USA, UK and Denmark, with a reduction of 15% in colorectal cancer mortality, but no impact on incidence. Overall screening with the FOBT test ensures a reduction in colorectal cancer mortality of 15%, reaching 23% when adjusted for individual attendance. The Guaiac FOBT is progressively replaced by a more specific immunochemical test (I-FOBT) based on human hemoglobin. Molecular markers of colorectal cancer, now developed through proteomics and genetics, should replace FOBT in the near future in organized screening protocols. DNA tests with a high sensitivity, based on molecular markers of the k-ras gene, are now available as stool tests 11. Circulating micro-RNAs also offer a large opening on easy screening with a simple blood sample 12. These tests, not yet cost-effective, are expected in the near future to replace in Mass Screening protocols the stool samples of FOBT by a simple blood sample.
Organized Mass Screening protocols with the FOBT test are proposed to the population of asymptomatic persons of both sexes in the age 50 to 70 years, by the Health Authorities, in the majority of Developed Countries in North America, Europe and Japan. As yet, the risk of colorectal cancer is lower in Developing Countries and Mass Screening protocols are considered as not justified; however, when the incidence increases in relation to development of the country the screening protocol should be developed. However, filter tests with molecular markers of cancer are still very costly, and it is unlikely that they will be deployed in Developing Countries.
3) Flexible Sigmoidoscopy: Flexible sigmoidoscopy explores distal large bowel with rectum and sigmoid. The procedure can also be performed by trained nurses. Guidelines on screening recommend that flexible sigmoidoscopy be repeated 5 years after an initial negative procedure. A cohort study conducted in 24,744 health professionals in the USA has shown that screening flexible sigmoidoscopy reduces mortality from colorectal cancer by 50%, and incidence by 44%.
In perspective, flexible sigmoidoscopy could offer a valuable protocol for colorectal cancer screening in Developing Countries classified by their G.N.I. in the Low Income group or in the Lower Middle Income group because of a better acceptance than colonoscopy and a lower cost.
4) Colonoscopy: is the gold standard procedure for the early detection of colorectal cancer and premalignant adenomatous polyps, which can be resected, preventing the later development of a cancer. The endoscopic destruction of premalignant precursors achieves a reduction of cancer incidence, as shown in the SEER registries of the USA 13: the ASR incidence/100 000, both sexes, decreased from 64.2 in 1985, to 60.6 in 1990 to 49.5 in 2003. Colonoscopy can be proposed in two situations:
a) As a primary procedure, without a filter test, in non organized, or “opportunistic screening”. In a group of average risk persons, aged 50 years or more, the yield of colonoscopy is under 1% for cancer, under 10% for advanced adenomas, and in the range 25 to 30% for all adenomas.
b) As a second procedure, performed after a positive filter FOBT in organized Mass Screening protocols. In the National Polyp study conducted in the USA the reduction of the risk of colorectal cancer in persons submitted to a colonoscopy was estimated at 75%.
Numerous screening trials have confirmed the reduction in mortality from colorectal cancer after colonoscopy, in spite of false negative procedures, resulting two or three years later in a so-called “interval” cancer 14,15. The endoscopic resection of adenomas has also an impact on the incidence of colorectal cancer. In the USA SEER Registries 13, during the period 1975/2003, the ASR incidence of colorectal cancer decreased by 19.4%, presumably as a consequence of the increased utilization of endoscopic treatment of their precursors.
Colonoscopy is currently performed in the More Developed countries in organized Mass Screening protocols in persons with a positive response to a filter FOBT. However compliance is limited, cost is high and there is a small toll of severe complications. In perspective, colonoscopy tends to be performed more often as a primary test in opportunistic non-organized screening for asymptomatic persons asking for prevention. In the USA colonoscopy every 10 years, from age 50 years is proposed without filter test as an alternative to Mass Screening. In addition Virtual colography with a 3D-multidetector scanner is an alternative to primary colonoscopy in non organized screening; however colonoscopy has to be performed when there is an abnormal finding.
In Developing Countries, the risk of colorectal cancer may increase, contrasting with a persistent weakness in organized Mass Screening, under control of Health Authorities. The discrepancy should encourage the growth of opportunistic indications for primary colonoscopy in spite of its high cost. However this is not a population-based strategy of prevention.
Conclusion on screening strategies
Implementation of screening measures in a country depends on Health Authorities, reimbursement facilities, and compliance of the population. In the Developed Countries of Europe and in Japan mass screening with the FOBT is proposed to the population and reimbursed, Germany and Italy also have organized screening protocols based on primary colonoscopy. Screening with primary sigmoidoscopy is encouraged in Scandinavian countries and in the UK with nurse endoscopists. In the USA the Medicare policy recommends annual FOBT or sigmoidoscopy every five years or colonoscopy every 10 years. In studies of the cost/effectiveness ratio, the screening of colorectal cancer is placed in the USA well under the financial benchmark adopted in screening ($40,000 per year of life gained). Developing countries with increasing resources should develop a policy of prevention of colorectal cancer based on population-based screening interventions with the less costly FOBT, and over time to primary endoscopy, with flexible sigmoidoscopy being the priority.
References
- Ferlay J, Shin HR, Bray F, Forman D, Mathers C, Parkin DM. GLOBOCAN 2008, Cancer Incidence and Mortality Worldwide: IARC CancerBase No. 10 . IARC Lyon; 2010. Available from: http://globocan.iarc.fr.
- Curado MP, Edwards B, Shin HR, Storm H, Ferlay J, Heanu M, et al. eds Cancer Incidence in Five Continents, Vol. IX, IARC Scientific Publications No. 160, IARC, Lyon, 2007 (and previous editions).
- World Bank list of economies (April 2012) at: http://shop.ifrs.org/files/CLASS.pdf and List of Countries by GDP (nominal) per capita. At http://en.wikipedia.org/wiki/.
- Coleman MP, Quaresma M, Berrino F, Lutz JM, De Angelis R, Capocaccia R, et al. Cancer survival in five continents: a worldwide population-based study (CONCORD). Lancet Oncol. 2008; 9: 730-56.
- Lund Nilsen TI, Vatten LJ. Colorectal cancer associated with BMI, physical activity, diabetes, and blood glucose. IARC Sci Publ. 2002; 156:257-8.
- Wolin KY, Yan Y, Colditz GA, Lee IM. Physical activity and colon cancer prevention: a meta-analysis. Br J Cancer. 2009; 100(4):611-6.
- Boffetta P, Couto E, Wichmann J, Ferrari P, Trichopoulos D, Bueno-de-Mesquita HB, van Duijnhoven FJ, et al.. Fruit, vegetables, and colorectal cancer risk: the European Prospective Investigation into Cancer and Nutrition. Am J Clin Nutr. 2009; 89:1441-52.
- Parkin DM, Boyd L, Walker LC. The fraction of cancer attributable to lifestyle and environmental factors in the UK in 2010. Br J Cancer. 2011;105 Suppl 2:S77-81.
- Sankaranarayanan R, Swaminathan R, Eds .Cancer survival in Africa, Asia, the Caribbean and Central America: IARC Scientific Publications N° 162, IARC, Lyon, 2011.
- Heresbach D, Manfredi S, D’halluin PN, Bretagne JF, Branger B. Review in depth and meta-analysis of controlled trials on colorectal cancer screening by faecal occult blood test. Eur J Gastroenterol Hepatol. 2006; 18:427-33.
- Imperiale TF, Ransohoff DF, Itzkowitz SH, et al. Fecal DNA versus fecal occult blood for colorectal-cancer screening in an average-risk population. N Engl J Med. 2004; 351:2704-14.
- Ahmed FE, Amed NC, Vos PW, et al.. Diagnostic microRNA markers to screen for sporadic human colon cancer in blood. Cancer Genomics Proteomics. 2012; 9:179-92.
- SEER Cancer Statistics Review, 1975- 2008, National Cancer Institute. Bethesda, MD, http://seer.cancer.gov/csr/1975_2008/.
- Brenner H, Chang-Claude J, Seiler CM, Hoffmeister M. Interval cancers after negative colonoscopy: population-based casecontrol study. Gut. 2012 Nov;61(11):1576-82.
- Steele RJ, McClements P, Watling C, et al. Interval cancers in a FOBT-based colorectal cancer population screening programme: implications for stage, gender and tumour site. Gut. 2012, 61, 576-581.